Sleep apnea is a sleep disorder defined by pauses in breathing or short breaths while sleeping. These disruptions, which can happen several times an hour, may disturb the body's regular sleep cycle and result in several health issues. At Beach Dental Care Anaheim, we provide remedies for sleep apnea, beginning with a complete assessment of your symptoms and risk factors. Our dentists collaborate closely with sleep specialists to guarantee an accurate diagnosis and a customized treatment strategy that meets your needs.
Types of Sleep Apnea
Although the most common kind is obstructive sleep apnea (OSA), there are additional varieties with unique traits and effects. Among them are:
Obstructive Sleep Apnea (OSA)
With obstructive sleep apnea making up about 84% of cases, it is the most common type of sleep apnea. It happens when the throat muscles relax significantly while asleep, which could block the airway completely or partially. This blockage causes breathing pauses, snoring, and disrupted sleep habits. Obesity, nasal congestion, and anatomic anomalies in the airway are common risk factors for OSA. If left untreated, OSA can increase the risk of heart problems, high blood pressure, memory loss, and exhaustion during the day.
Central Sleep Apnea (CSA)
Compared to OSA, central sleep apnea is less common and is caused by a malfunction in the respiratory control centers of the brain. In contrast to OSA, in which breathing pauses are mostly caused by airway obstruction, CSA arises from the brain's inability to properly communicate with the breathing muscles. People who have CSA consequently go through phases of shallow or nonexistent breathing when they sleep. Heart failure, stroke, and neurological problems are among the underlying medical issues that are frequently linked to CSA. Symptoms could include breathing difficulties, trouble falling asleep, and nocturnal awakenings. In addition to treating the underlying medical issue, treatment for CSA may entail adaptive servo-ventilation or supplemental oxygen therapy.
Complex Sleep Apnea Syndrome
The combination of central and obstructive sleep apnea symptoms is called complex sleep apnea syndrome, or treatment-emergent CSPA. After beginning continuous positive airway pressure (CPAP) therapy, people with complicated sleep apnea acquire central sleep apnea, while initially exhibiting symptoms that correspond to OSA. Although the exact causes of complicated sleep apnea syndrome are unknown, it is thought that changes in respiratory control and anatomical factors combine extensively. Using adaptive servo-ventilation devices, modifying CPAP settings, or, in some cases, considering surgical procedures are some of the treatment options for complicated sleep apnea.
Symptoms of Sleep Apnea
Some of the most common signs of sleep apnea are listed below:
Loud and Persistent Snoring
A common sign of sleep apnea is loud, continuous snoring. As snoring on occasion is normal and may not always be a sign of a sleep problem, heavy snoring combined with gasping or choking sounds as you sleep can often be a sign of obstructive sleep apnea (OSA). When throat muscles are loose, airflow becomes restricted, causing vibrations of the soft tissues in the airway and the sound of snoring.
Pauses in Breathing
Sleep apnea patients may encounter apneas, or breathing pauses, while they are asleep. As breathing continues, there may be choking or gasping sensations during these breathing pauses, which can last anywhere from a few seconds to a minute or longer. Family members or bed partners may detect the changes in the person's respiratory patterns, even though the person may not always be conscious of these episodes.
Daytime Fatigue and Sleepiness
A common sign of sleep apnea is excessive daytime sleepiness and weariness, which is caused by fragmented sleep and insufficient rest during the night. Even after getting enough sleep, people with sleep apnea may wake up feeling rested and find it difficult to stay awake or focused during the day. Daytime weariness might affect one's ability to think clearly, focus, and perform well at work or school.
Morning Headaches
Another common sign of sleep apnea is morning headaches, which are frequently linked to changes in oxygen saturation and carbon dioxide retention as you sleep. People may experience a dull, throbbing headache upon waking up, which may become better over time. Morning headaches may be accompanied by irritation, mood fluctuations, and difficulties concentrating..
Nocturnal Urination (Nocturia)
Patients with sleep apnea often experience nocturia or frequent overnight urine. Breathing pauses and waking up can disturb sleep, which might increase the production of urine and necessitate nighttime urination. Nocturia can exacerbate sleep disruption and increase drowsiness and weariness during the day.
Other Symptoms
A decrease in libido or sexual dysfunction are possible side effects of sleep apnea, along with restless sleep, irritation, mood swings, dry mouth or sore throat upon awakening. Symptoms of sleep apnea in children can include bedwetting, poor academic performance, hyperactivity, or behavioral issues.
Exploring the Causes of Sleep Apnea
Some common causes of sleep apnea include:
Obesity
Obstructive sleep apnea (OSA), the most prevalent kind of sleep apnea, has obesity as a major risk factor. It can become more difficult to breathe while you sleep if you have excess fat deposits around your throat and neck. Snoring, breathing pauses, and irregular sleep patterns can be caused by the increased pressure on the airway. Weight loss is frequently advised as part of the treatment strategy to reduce symptoms and enhance sleep quality because obese people are more likely to develop OSA.
Anatomical Factors
A person may be predisposed to sleep apnea by anatomical abnormalities in the upper airway. Narrow airways, big tonsils or adenoids, a large tongue, or a deviated septum are examples of common structural problems. These structural differences may be involved in airway blockage during sleep, which can cause breathing problems and disrupt sleep. The diagnosis of sleep apnea and the choice of suitable treatment options, such as oral appliances or surgical procedures, depend on the assessment of the upper airway anatomy using imaging investigations or physical examination.
Age
Elderly persons are more susceptible to sleep apnea due to age-related changes in muscle tone and tissue flexibility. The airway-supporting muscles may weaken with age, making the throat more likely to collapse while you sleep. Furthermore, medical disorders like obesity, heart disease, and hypertension are more common in older persons and are linked to an increased risk of sleep apnea. Frequent screening for sleep apnea in the elderly population, in conjunction with the treatment of underlying medical disorders, can help lessen the negative effects of aging on breathing and sleep quality.
Genetics
Research indicates that there may be a hereditary component to sleep apnea, as the disorder appears to run in families. An increased likelihood of developing sleep apnea is linked to a family history of the condition, suggesting a possible genetic component. Sleep apnea etiology may be influenced by genetic changes in airway morphology, respiratory control systems, or metabolic factors. Knowing the genetic foundation of sleep apnea can help develop tailored treatment plans that focus on particular genetic pathways or risk factors.
Lifestyle Habits
Some lifestyle choices, like drinking alcohol, smoking, and using sedatives, can make sleep apnea worse and hasten its development. Smoking can aggravate fluid retention and inflammation in the airways, which can constrict and clog them. Alcohol and sedatives cause the throat muscles to relax, which worsens respiratory health and airway patency as you sleep. A healthy lifestyle that includes regular exercise, cutting back on alcohol use, and quitting smoking might help lessen the severity of sleep apnea and enhance overall sleep quality.
Diagnosis of Sleep Apnea
Sleep apnea is diagnosed using a combination of clinical examination, sleep testing, and symptom assessment. This is an outline of the diagnostic procedure:
Clinical Assessment
First, your healthcare professional will perform a complete physical examination and take your medical history. They will ask you about your symptoms, sleeping habits, health issues, prescription drugs, and way of life.
Be ready to talk about any signs that are related to sleep apnea, like excessive snoring, feeling like you're gasping or choking as you sleep, exhaustion during the day, headaches in the morning, agitation, and trouble focusing.
Sleep Questionnaires
You may be requested to fill out sleep questionnaires or surveys to provide further information about your sleeping habits and daytime functioning. These tests assist in determining how severe your symptoms are and how they affect your overall well-being.
The Polysomnography Sleep Study
The gold standard for identifying sleep apnea is polysomnography. This extensive sleep study is carried out in a sleep laboratory, although portable monitoring devices can also be used at home.
When you sleep during a polysomnography, a number of physiological markers are tracked, such as:
- Brain waves (electroencephalography, EEG).
- Eye movements (electrooculography, EOG).
- Muscle activity (electromyography, EMG).
- Heart rate and rhythm (electrocardiography, ECG).
- Breathing patterns (nasal airflow, respiratory effort).
- Oxygen saturation levels (pulse oximetry).
Using polysomnography, medical professionals can evaluate the frequency and severity of oxygen desaturation episodes, breathing irregularities, and changes in sleep architecture that are indicative of sleep apnea.
Home Sleep Apnea Testing (HSAT)
Your healthcare physician may occasionally suggest home sleep apnea testing as a more practical and affordable option to polysomnography, particularly in situations of simple obstructive sleep apnea (OSA) in people without substantial comorbidities.
HSAT requires you to wear a portable monitoring device while you sleep at home. In order to identify breathing irregularities suggestive of sleep apnea, the device monitors factors like airflow, respiratory effort, oxygen saturation, and heart rate.
Does Sleep Apnea Have a Cure?
Although there isn't a permanent cure for sleep apnea, symptoms can be effectively managed with treatment, which can also enhance quality of life. Continuous positive airway pressure (CPAP) therapy, dental appliances, lifestyle changes, and, in certain situations, surgical procedures can all be helpful in the long-term management of sleep apnea. People with sleep apnea can experience symptom alleviation, lower health risks, and rejuvenating sleep by treating underlying risk factors, improving treatment adherence, and collaborating closely with healthcare providers.
Treatment Options for Sleep Apnea
Although there is no known cure for sleep apnea, there are a number of ways to manage symptoms, enhance sleep quality, and lower the risks associated with the condition.These treatment options include:
Continuous Positive Airway Pressure (CPAP) Therapy
CPAP therapy, which is the main treatment for moderate to severe obstructive sleep apnea (OSA), involves wearing a mask that is connected to a machine that continuously streams air into the airway to keep it open while you sleep. It works by preventing airway collapse, reducing the frequency of apneas and hypopneas, and improving both the quality of sleep and daytime functioning. However, in order to get the best results, CPAP therapy must be used consistently and appropriately.
Oral Appliances
Mandibular advancement devices, or oral appliances, are specially designed mouthpieces that realign the lower jaw and tongue to avoid obstructing the airway as you sleep.
For people with mild to moderate OSA or those who are unable to tolerate CPAP therapy, oral appliances are appropriate. Most patients find them to be well-tolerated, pleasant, and simple to use.
Lifestyle Modifications
- Loss of weight — One of the main risk factors for sleep apnea is being overweight. Even a small weight loss can lessen the severity of sleep apnea and alleviate symptoms.
- Avoid alcohol and sedatives — These substances can relax the throat muscles, making airway collapse during sleep worse. Reducing or eliminating these substances prior to going to bed can help with the symptoms of sleep apnea.
- Positional therapy — For some people with positional OSA, sleeping on one's side rather than on one's back (supine position) may assist avoid airway obstruction.
Surgery
If a patient with severe OSA is unable to use CPAP therapy or has not responded to conservative therapies, surgical techniques may be considered.
Uvulopalatopharyngoplasty (UPPP), tonsillectomy and adenoidectomy, maxillomandibular advancement (MMA) surgery, and hypoglossal nerve stimulation are among the surgical techniques available for treating sleep apnea.
Who Is More Prone to Sleep Apnea?
The following are some of the factors that raise the risk of sleep apnea among particular populations:
Older Adults
Aging is a major risk factor for sleep apnea, particularly obstructive sleep apnea (OSA). Age-related changes in tissue elasticity and muscle tone may increase the risk of airway blockage or collapse as you sleep. Obesity, hypertension, and cardiovascular disease are age-related diseases that also contribute to the higher rates of sleep apnea in the elderly. Moreover, age-related alterations in the architecture of sleep, such as decreased REM and deep sleep, can aggravate the symptoms of sleep apnea and lower the standard of overall sleep.
Individuals with Obesity
Obesity is a major risk factor for sleep apnea, as excess weight causes airway narrowing or obstruction during sleep. Fat deposits accumulating in the neck and throat can restrict the airway, causing apneas and snoring, among other breathing disorders. Individuals who are obese have a greater risk of sleep apnea than people who are normal weight. Therefore, treating obese people with sleep apnea often involves weight management measures.
Individuals with Anatomical Abnormalities
People who have larger tonsils or adenoids, a narrow airway, or a large tongue are more likely to have airway obstruction while they sleep, which puts them at risk for sleep apnea. These anatomical abnormalities may cause breathing and airflow obstructions, which may result in breathing pauses, snoring, and disrupted sleep habits. Certain populations, such as kids and those with craniofacial defects, are more likely to have anatomical abnormalities. These populations may need specific interventions in order to effectively manage the symptoms of sleep apnea.
Individuals with a Family History
Genetic factors may impact airway morphology, respiratory control systems, or metabolic processes involved in sleep apnea etiology. People who have a family history of sleep apnea should be on the lookout for symptoms and should get checked out by a doctor if they do.
Health Implications of Untreated Sleep Apnea
If left untreated, sleep apnea presents serious threats to general health and well-being in addition to interfering with restorative sleep.
Cardiovascular Diseases
Untreated sleep apnea is associated with an increased risk of cardiovascular disorders such as hypertension, coronary artery disease, and stroke. The recurrent episodes of oxygen desaturation and sleep pattern abnormalities linked to sleep apnea can cause inflammation, high blood pressure, and endothelial dysfunction, which can aid in the onset and advancement of cardiovascular diseases. Individuals with untreated sleep apnea are more likely to suffer heart attacks, arrhythmias, and other cardiovascular problems than those without the illness.
Hypertension
Hypertension and sleep apnea often combine, creating a risky cycle that raises cardiovascular risk. Blood pressure spikes and nocturnal hypertension are caused by the sympathetic nervous system being activated by recurrent episodes of apnea and hypopnea during sleep. Untreated sleep apnea raises the risk of hypertension and its side effects, including heart failure, renal disease, and stroke, over time by causing prolonged blood pressure increases.
Metabolic Disorders
Untreated sleep apnea is linked to metabolic abnormalities, insulin resistance, and an increased risk of type 2 diabetes. People with sleep apnea often have fragmented sleep patterns and intermittent hypoxia, which can interfere with insulin sensitivity, affect glucose metabolism, and increase oxidative stress and inflammation. Thus, untreated sleep apnea may increase the risk of metabolic diseases by fostering their emergence and exacerbation, as well as by increasing the likelihood of cardiovascular problems and other health problems
Neurocognitive Impairments
Sleep apnea can impair cognitive performance, mood regulation, and daily functioning owing to sleep fragmentation and chronic sleep deprivation. Cognitive impairments, such as deficiencies in attention, memory, executive function, and psychomotor performance, are linked to untreated sleep apnea. Daytime tiredness, excessive drowsiness, irritability, mood swings, and poor focus can all severely affect an individual's ability to function at work, in school, and in daily life.
Daytime Functioning and Quality of Life
Untreated sleep apnea can have a severe impact on daytime functioning, productivity, and quality of life. In addition to lowering general well-being and quality of life, chronic sleep deprivation and daytime sleepiness can impede cognitive function and raise the risk of accidents and injuries. The influence of sleep abnormalities on mental health and functioning can lead to mood disorders, social and vocational challenges, and worsened interpersonal interactions in those with untreated sleep apnea
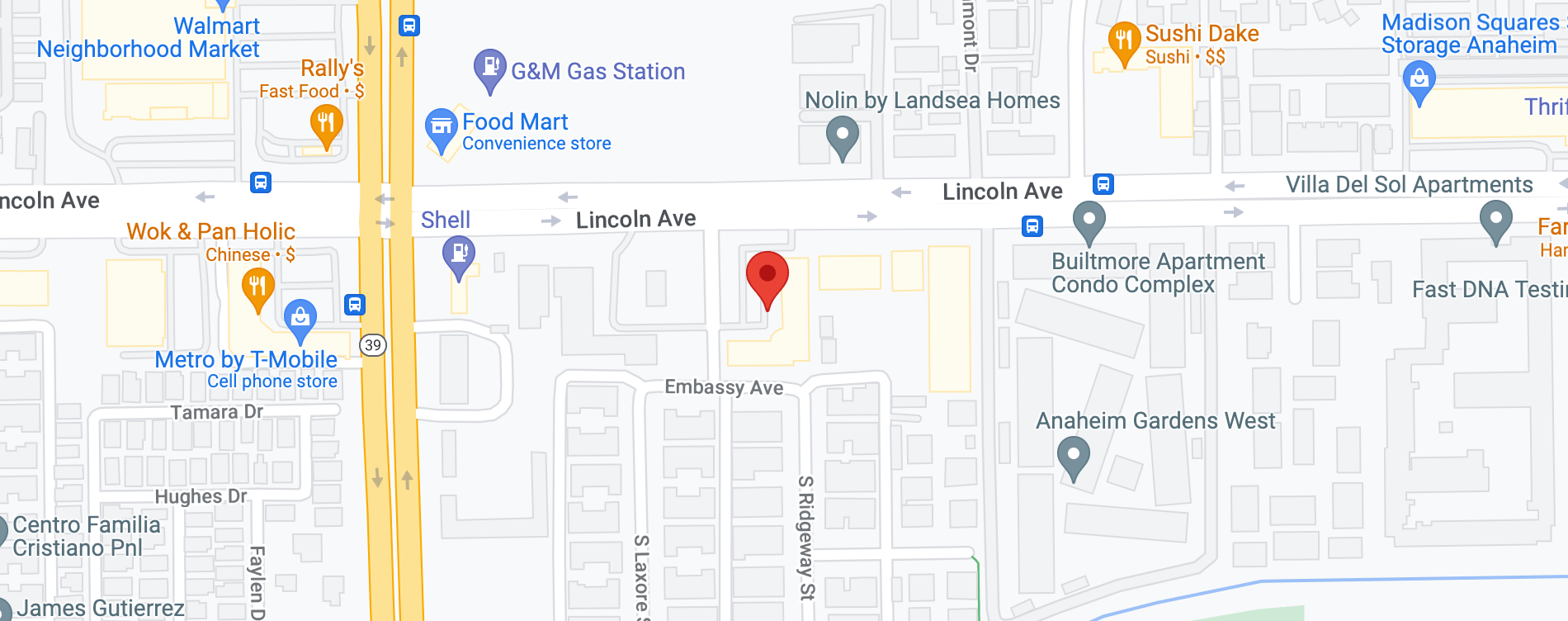
Find a Dental Care Specialist Near Me
Sleep apnea should not be left untreated. If you believe you have this condition or are experiencing symptoms of sleep apnea, contact Beach Dental Care Anaheim immediately to schedule a consultation. We can collaborate with you to discover practical solutions that will enable you to get a good night's sleep and improve your general health. Give us a call at 714-995-4000 today.